Two independent proteomic approaches provide a comprehensive analysis of the synovial fluid proteome response to Autologous Chondrocyte Implantation
Abstract
Background: Autologous chondrocyte implantation (ACI) has a failure rate of approximately 20%, but it is yet to be fully understood why. Biomarkers are needed that can pre-operatively predict in which patients it is likely to fail, so that alternative or individualised therapies can be offered. We previously used label-free quantitation (LF) with a dynamic range compression proteomic approach to assess the synovial fluid (SF) of ACI responders and non-responders. However, we were able to identify only a few differentially abundant proteins at baseline. In the present study, we built upon these previous findings by assessing higher-abundance proteins within this SF, providing a more global proteomic analysis on the basis of which more of the biology underlying ACI success or failure can be understood.
Methods: Isobaric tagging for relative and absolute quantitation (iTRAQ) proteomic analysis was used to assess SF from ACI responders (mean Lysholm improvement of 33; n=14) and non-responders (mean Lysholm decrease of 14; n=13) at the two stages of surgery (cartilage harvest and chondrocyte implantation). Differentially abundant proteins in iTRAQ and combined iTRAQ and LF datasets were investigated using pathway and network analyses.
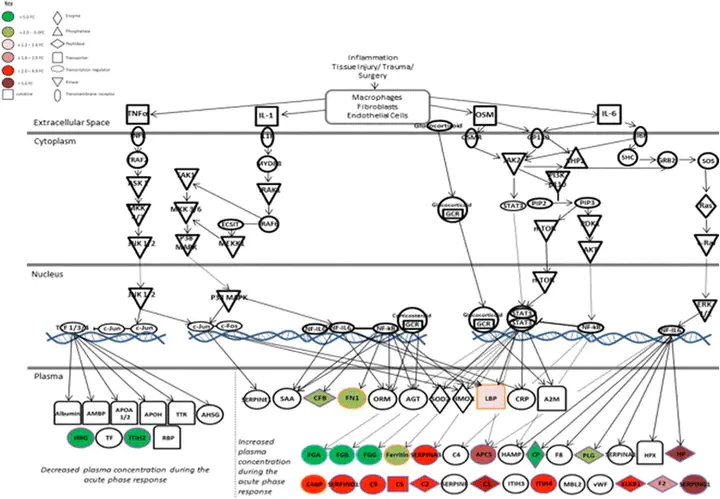
Results: iTRAQ proteomic analysis confirmed our previous finding that there is a marked proteomic shift in response to cartilage harvest (70 and 54 proteins demonstrating ≥2.0-fold change and p<0.05 between stages I and II in responders and non-responders, respectively). Further, it highlighted 28 proteins that were differentially abundant between responders and non-responders to ACI, which were not found in the LF study, 16 of which were altered at baseline. The differential expression of two proteins (complement C1s subcomponent and matrix metalloproteinase 3) was confirmed biochemically. Combination of the iTRAQ and LF proteomic datasets generated in-depth SF proteome information that was used to generate interactome networks representing ACI success or failure. Functional pathways that are dysregulated in ACI non-responders were identified, including acute-phase response signalling.
Conclusions: Several candidate biomarkers for baseline prediction of ACI outcome were identified. A holistic overview of the SF proteome in responders and non-responders to ACI has been profiled, providing a better understanding of the biological pathways underlying clinical outcome, particularly the differential response to cartilage harvest in non-responders.