Does knee cartilage repair surgery prevent arthritis or the need for a joint replacement?
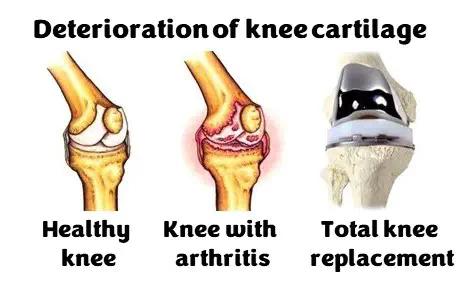
Musculoskeletal conditions, such as arthritis, account for 20% of GP visits. Arthritis is a wide-spread disease which affects our joints, and osteoarthritis (OA) is the most common form. In the UK, approximately 1/5 of over-45s have been diagnosed with OA, the knee being the most frequently affected joint. The cause of OA is unknown but it develops when cartilage wears out. Knee injury in young adults can increase their risk of developing knee OA sixfold. OA is treated with physiotherapy, painkillers, surgery, or as a last resort, a joint replacement.
Cartilage repair surgeries focus on stopping knee pain and improving function but may also slow OA. It’s important to measure outcomes following surgery to understand if they have worked. There are different ways to assess outcome for knee cartilage surgery including clinical (e.g., need for re-operation or joint replacement), X-rays, cartilage or bone tests, studying genes or proteins in blood samples, or ‘patient reported’ (e.g., questionnaires). Outcomes are collected and stored in large health databases and registries.
Ideally, knee cartilage surgeries in middle-aged patients will slow down OA and delay or eliminate the need for joint replacement. We don’t know if this happens in reality. I plan to work out the true effect of knee cartilage surgeries by studying health records and outcome measures.
The Robert Jones & Agnes Hunt Orthopaedic NHS Hospital in Oswestry specialises in bone and joint disorders. Uniquely, it has cartilage surgery data spanning more than 20 years. I plan to link this information with the National Joint Registry (results from joint replacements) to work out the time from surgery to joint replacement to see if I can predict when and for whom cartilage surgery would be successful. Also, I plan to use the UK Biobank (health records and risk factors for the major diseases of middle and old age) to find out whether cartilage surgery can help patients with a higher genetic risk of OA onset.
The study will help patients with cartilage defects by giving orthopaedic surgeons a tool to help fit cartilage treatment to their patients to delay or avoid the development of severe OA. This will improve their quality of life and reduce the need for knee replacements, both of which represent health-economic benefits. This potential cost benefit also fits with the NHS national programme “GIRFT” (https://gettingitrightfirsttime.co.uk/).